How Your Gut Microbiome Affects Your Oxalate Tolerance
June 23, 2024 | Source: Mercola.com | by Dr. Joseph Mercola
Oxalates are naturally occurring substances found in many plants, including vegetables, fruits, nuts and seeds. Chemically, oxalate is the ionized form of oxalic acid, explains Ruth Ann Foster, ScD, BSN, RN.1 While they’re a normal part of human metabolism and your diet, they can bind to minerals like calcium, forming crystals known as calcium oxalate.
When consumed in large amounts or in susceptible individuals, oxalates can contribute to the formation of kidney stones. However, the problem isn’t the oxalates themselves but a damaged gut, which interferes with your body’s ability to clear oxalates effectively.
In my interview with Foster, who has a doctorate in holistic nutrition and studies the relationships between minerals, microbes and water, we explore the underlying causes of that gut dysfunction and how it relates to overall health.
People Have Eaten High-Oxalate Diets for Millenia
“I really got started on oxalates when I was doing my dissertation on magnesium and drinking water. And because magnesium is, you know, vital it inside the cell,” Foster explains. “It’s an antagonist with calcium, which is made mainly outside of the cell. And, you know, the majority of kidney stones are calcium oxalate, and that has coincided with a deficiency in magnesium. So, I was well aware of problems with oxalates.”2
However, she started to wonder why oxalates are such a problem. Initially, she thought plants may be the issue, assuming Eskimos and other native cultures didn’t eat a lot of high-oxalate foods and were therefore healthy, with low rates of kidney stones. But it turned out that high-oxalate foods are common in many traditional diets:3
“I found that there are a lot of ancestral tribes and communities that ate a lot of oxalates and a lot of people that are still living on them today. So, then I started looking more into kidney stone disease and realize yes, while it’s been around since antiquity, it really has taken off exponentially since the Industrial Revolution — since we started eating processed foods.
And, you know, processing our water to take the magnesium out of the drinking water … one of the first groups of people that I looked at … were the people in the lower Pecos … region of I think it’s Western Texas, and they ate a lot of oxalates. But they were able to clear them.
And then looking around at that, looking at animals in the kind of desert area, there’s a wood rat, a white-throated wood rat, that also consumes most of its diet in an oxalate cactus and things like that. But it also excretes them.
So, scientists are now using the woodrat to study our microbiome. And they’ve taken some of the transplanted fecal material from the woodrat into lab rats. And they’ve been able to maintain oxalate clearing tolerance for nine months later. So, there’s something going on in the gut microbiome.”
Foster also researched the Inuits, first assuming that their very low rates of kidney stone disease are due to a diet low in fruits and vegetables, and low in oxalates. Yet, once again, she revealed these native cultures have eaten high-oxalate foods all along, without the problems they cause to so many people today:4
“It turns out … the Inuits eat a lot of high-oxalate foods, and they eat them all year long. They don’t just eat them [during] their short little growing season. They ferment them, they dry them, and so on …
Plus, the other thing that they would do is they eat the rumen of some of the reindeer that they find, which is, again, it’s going to have some bacteria in it. And that helps them to be able to process through these things. So then looking at Africa, same kind of thing, high-oxalate foods. And in each one of these situations, all of these people have been able to clear the oxalates.”
Antibiotics, Ultraprocessed Foods Are Destroying Gut Health
Exposures to antibiotics and ultraprocessed foods represent a key difference in traditional cultures and those living in the modern world. These factors are destroying gut health among those living in the Western world, such that many people are unable to handle high-oxalate foods.
“Overall, accumulating evidence reveals that kidney stones are fundamentally linked to a damaged gut, which impairs the body’s ability to clear oxalates. We must, therefore, consider the real culprits like refined sweeteners, ultraprocessed foods and seed oils — hallmarks of the modern industrial diet,” Foster writes.5
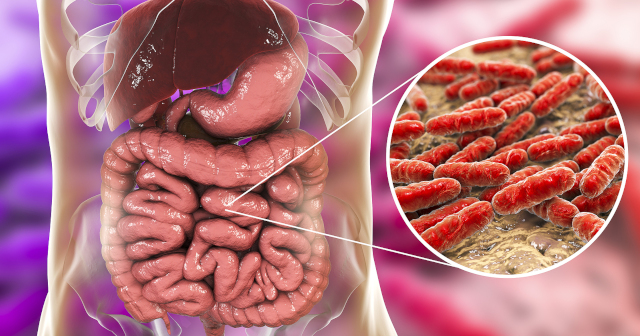
One consequence is that an important bacterium, Oxalobacter formigenes, is now missing in many adults’ guts. “A lot of the primitive cultures still have Oxalobacter in their guts,” Foster says.6 This beneficial bacterium plays a crucial role in the metabolism and regulation of bodily oxalate levels. It digests oxalate crystals and basically signals the gut wall to excrete oxalate for its own nourishment.
In this way, Oxalobacter helps reduce the concentration of oxalate in your gut, which can consequently lower the risk of oxalate crystallization and the formation of kidney stones and other health problems. However, this is just one type of beneficial bacteria involved in oxalate degradation. According to Foster:7
“With rapid advances in technology, scientists have learned that multiple bacterial species can degrade oxalate, working through a large network. For example, monitoring the gut bacteria of over one thousand healthy participants, one study found that the majority (92%) of gut microbiomes contained several species of oxalate-degrading bacteria.
Because of the complexity of the oxalate-degrading network, researchers now understand the importance of assessing gut health in its entirety rather than focusing on a single bacterial type such as O. formigenes … Hence, a healthy gut is key to maintaining oxalate tolerance.”
Healthy Foods Often Get Blamed for Problems Caused by a Damaged Gut
Often, Foster says, when people try to switch from a highly processed diet to a healthy one, they introduce more high-oxalate foods, like spinach and beets. Then, digestive issues, such as bloating, gas and abdominal pain, may occur due to the irritation of the intestinal lining by oxalates.
“You want to correct it and so you start eating healthy, and then you get even sicker … then, instead of blaming the bad foods, you blame the healthy food,” Foster says. In short, as a result of an ultraprocessed diet, mitochondrial dysfunction and an inability to create sufficient cellular energy occurs.
So, many people have lost the ability to maintain a high enough concentration of beneficial bacteria in their gut that actually digest the healthy fibers in fruit, vegetables and grain. Then, when you do eat those types of foods, you get worse, as you’re not feeding the good bacteria anymore, because they’re not there, they can’t survive.
Instead, you have a buildup of pathogenic bacteria that produce toxic endotoxin, one of several factors that destroys mitochondrial function.
Two Major Types of Bacteria — Oxygen Tolerant and Oxygen Intolerant
A healthy gut with a properly maintained anaerobic environment supports the growth of beneficial oxygen intolerant, such as the keystone species Akkermansia. When the oxygen gradient is disturbed due to insufficient energy production (as seen in metabolically inflexible individuals), it allows pathogenic oxygen tolerant bacteria to proliferate.
These bacteria often produce more virulent endotoxins, also known as lipopolysaccharides (LPS), which can cause inflammation if they translocate across the compromised gut barrier into the systemic circulation. Oxalates indirectly contribute to this scenario by exacerbating mitochondrial dysfunction and reducing cellular energy production.
Colonocytes are the epithelial cells lining the surface of your colon, where they make up the majority — about 80% — of the epithelial cell population. Not only do they serve as the barrier, the actual lining of your gut, but they perform beta oxidation and are involved in the metabolism of short chain fatty acids.
In the process of metabolizing short chain fatty acids, colonocytes consume a significant amount of oxygen, reducing the oxygen levels in your colon. The short chain fatty acids that colonocytes need are produced from the fibers that you eat — typically from healthy foods like vegetables, apples and other fruits.
These fibers nourish both good and bad bacteria, however. if you have a preponderance of pathogenic bacteria, it makes it hard to eat healthy, because eating healthy foods makes you feel worse due to the radical increase in endotoxin, which can kill you.
In my view, the No. 1 cause of death, that exceeds heart disease and cancer, is endotoxemia. Healthy, unprocessed foods are historically all our ancient ancestors had — they didn’t have to deal with processed foods. So, they had a healthy gut and were able to consume high-oxalate foods without a problem.
Once your gut is healthy, consuming dietary oxalate helps you maintain tolerance by feeding sustaining oxalate-degrading bacteria, Foster notes. The key is to consume a healthy amount — neither too much nor too little:8
“Maintaining tolerance by daily consuming some dietary oxalate is important. Ironically, when dietary oxalate intake is lower than fifty milligrams per day, oxalate absorption increases significantly. At the same time, overconsuming high amounts of dietary oxalates, especially in the form of foods like spinach smoothies, can be hazardous.”
As mentioned, you have to have cellular energy to consume high-oxalate foods without issue. But if you don’t have it, then you enter a cascading downhill spiral that gets increasingly worse.
Modern Diets Are the Problem
Foster points out that it’s not dietary oxalates that are the issue, but rather modern diets focused on ultraprocessed foods:9
“Considering escalating diabetes rates and poor American dietary habits, it appears that gut dysbiosis and the overconsumption of industrially ultraprocessed foods are more responsible for oxalate toxicity than the overconsumption of so-called ‘superfoods’ like spinach or sweet potatoes.
Simply put, it is not oxalate-containing foods like spinach that are increasing the production and absorption of oxalate. To address the oxalate problem, we must consider the impact of processed and ultraprocessed industrial foods on gut and kidney health.”
This includes seeds oils, high in omega-6 polyunsaturated fatty acids (PUFAs) like linoleic acid. Foster explains:10
“Overconsumption of industrial seed oils, high in omega-6 polyunsaturated fatty acids (PUFAs), contributes to AGE [advanced glycation end product] production … The fatty acid ratio of omega-6 to omega-3 is a driving factor in kidney disease and many other chronic illnesses.
In the past 30 years, dietary omega-6 consumption has increased in the face of omega-3 deficiency. The ideal ratio of omega-6 to omega-3 is about two to one, but today’s ratio is over 20 to one. Researchers have noted that a ‘USDA egg’ has an omega-6 to omega-3 ratio of about 20:1.
Industrial seed oils and other sources of omega-6 weaken and soften the cell membranes, which enhance oxalate binding to the nephrons and begin crystal formation. Accumulating evidence shows a link between increased consumption of omega-6 fatty acids and kidney stone disease.
In contrast, higher intakes of omega-3 fatty acid (mostly from seafood) protect against the risk of kidney stone formation, CKD [chronic kidney disease] and other degenerative diseases, as evidenced by the diet of traditional Inuit populations, rich in omega-3 fatty acids.”
The addition of excessive amounts of omega-6 fat to the diet via ultraprocessed foods is what catalyzed the now epidemic levels of mitochondrial dysfunction. It caused depletion of colonocytes because of the gradual intrusion and increase in oxygen concentration in the colon that causes this cascade of death in your microbiome.
Glucose (Dextrose) May Offer a Short-Term Solution
In my view, the healthiest fuel for your mitochondria is glucose, not fat, as fat increases reductive stress and slows down the electron transport chain. Some cells, like the colonocytes, thrive on beta oxidation, so do our heart cells. Most cells require glucose, but if you’re following a keto or carnivore diet, you’re likely carb deficient.
There’s a lot of consequences from that, but many people get better on carnivore or keto because they stop eating ultraprocessed foods and feeding these patterns.
In the short-term, however, to get out of this destructive cycle, consider taking glucose, which is more commonly called dextrose. It’s pretty inexpensive — about $5 a pound. Glucose never reaches your colon; it’s all absorbed in your small intestine. Because of that, it avoids the complication of providing fuel to the facultative anaerobes, the pathogenic bacteria that can make endotoxin.
Consuming glucose is preferable to not consuming any carbs, which is highly problematic, in part because your cortisol level goes up. Ultimately, if your body is producing high amounts of cortisol to compensate for the lack of healthy carbs in your diet, this is not a state you want to be in for a prolonged period if you want to live a long and healthy life.
So, if you’re unable to tolerate healthy carbs, try pure glucose for a few weeks. This is especially useful for those who are seriously damaged, who don’t have the capacity to eat virtually any carbohydrates. You can go on a high-dextrose diet until your gut starts to heal. You save more cellular energy, which allows you to introduce more carbs back in to your diet, helping to restore your mitochondrial function.
Fraud in the Probiotics Market
Unfortunately, once you’re lacking cellular energy and your gut health is disrupted, most probiotic supplements on the market are useless, as they’re all fatally flawed. No one has yet figured out how to how to take that raw material and put it in a capsule and get it into your gut. It dies in the meantime. There’s a lot of fraud going on in this area, which I’m going to expose shortly.
Further, no one has yet grown Oxalobacter, but I’ve got a research team on it right now to define the protocol. These bugs are very difficult to grow and require many millions of dollars of investment to identify the specific protocol that causes them to thrive and then to harvest them. Once they’re harvested, you still have the technical challenge of putting them into a capsule in a way that doesn’t kill them.
I’m hoping we’ll have Oxalobacter within a year or two. It’s one of our priorities to get that out because it’s just like a seed to encourage good bacterial growth in your gut. But remember, if you put a seed in the Sahara Desert, and there’s no water, the seed can’t grow. It’s the same with Oxalobacter.
Even if you have the best Oxalobacter supplement in the world, if you put it in most everyone’s gut, nothing’s going to happen because the environment isn’t healthy enough to support it. You have to take care of the foundational causes of the issue first, including resolving mitochondrial dysfunction and an inability to create sufficient cellular energy.
Protecting Your Microbiome Is Key
The health of your microbiome begins even before birth, from conception. This crucial window of development sets the stage for your gut health — a topic Foster says she’d like to expand on in book form:11
“The book that I would like to write is … the first 1000 days. And it is from conception to about age 3, when that whole microbiome is developed … we get our gut colonized at birth … we [once] thought that the baby was born sterile. We now know that babies come out with, I think, 100 different species in the colon, ready to go. And it comes from the mother’s … microbiome.”
However, early antibiotic treatments, lack of breastfeeding and other factors often disrupt gut microbiome early on. At any age, however, promoting a healthy gut microbiome by avoiding ultraprocessed foods and consuming probiotic-rich foods like yogurt, kefir and fermented vegetables can support the growth of beneficial bacteria, including those that can degrade oxalates like Oxalobacter.
Drinking sufficient water is also crucial as it helps to flush out oxalates through your urine and prevents kidney stones from forming. Foster explains that not only is the quality of your drinking water important but the mineral content also matters:12
“Higher mineral content is associated with increased urinary citrate, while lower mineral content is not. Mineral water frequently contains bicarbonate, which is absent in tap water. Gerolsteiner, a naturally sparkling mineral water, is a great source of magnesium and high in bicarbonate. As mentioned, magnesium is a natural stone inhibitor, while bicarbonate increases the excretion of citrate, another important inhibitor.
Mineral water provides the most bioavailable forms of magnesium and calcium. Because they are hydrated (ionic), these minerals are rapidly absorbed. Likewise, raw milk is a valuable source of bioavailable magnesium and calcium. Other liquids to increase hydration can include bone broths, soups, tea (depending on oxalate content) and limited amounts of sour kombucha.”
References
